Fiji’s Hidden Paradise Turns Crisis Zone
Fiji, often celebrated as a postcard-perfect tourist paradise, is now the focus of grim global headlines. The Fiji HIV crisishas reached unprecedented levels, forcing the government to declare a formal outbreak in January 2025. For a small island nation with limited healthcare infrastructure, the scale of this epidemic is staggering. Experts warn that it has become one of the fastest-growing HIV epidemics in the world, with lessons that extend far beyond the Pacific.
For years, Fiji was rarely mentioned in the same breath as HIV hotspots. But today, international agencies, health experts, and regional governments are all paying close attention. The speed of the outbreak is not only destabilizing Fiji’s healthcare system—it is also reshaping how the world views the risks of injecting drug use in places once thought relatively safe.
From Low Prevalence to Alarming Growth
In 2014, Fiji had fewer than 500 people living with HIV. A decade later, UNAIDS estimates show that number has surged to around 5,900, with upper estimates as high as 8,900. This exponential growth marks a fundamental shift: from low-level prevalence to full-blown emergency.
Several forces collided to create the HIV crisis in Fiji:
- Methamphetamine trafficking and use: Syringes filled with meth are openly sold in Suva, normalizing injection drug use among younger populations.
- System unpreparedness: Fiji’s health services were built around preventing sexual transmission of HIV, not drug-related epidemics.
- Stigma and misinformation: Fear of discrimination keeps many away from testing centers, while myths fuel risky practices.
- Absence of harm-reduction programs: Unlike many countries, Fiji has not yet implemented large-scale needle–syringe programs or opioid substitution therapy.
Together, these gaps allowed high-risk practices to spread unchecked, culminating in today’s Fiji HIV crisis.
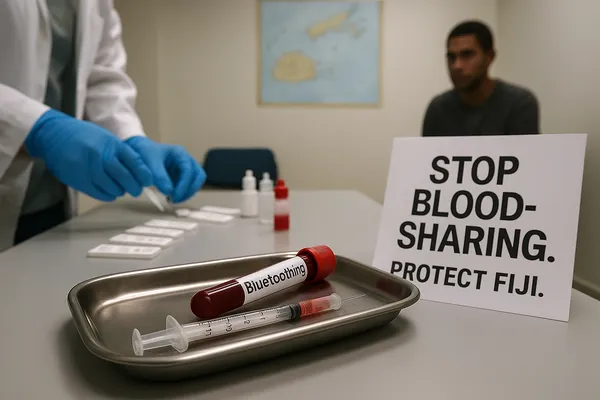
The Dangerous Practice of Blood-Sharing
The single most alarming factor driving this epidemic is “bluetoothing,” or blood-sharing. After injecting meth, one user draws their blood into a syringe and passes it to another person. That individual injects the blood directly into their veins.
Health experts warn this is catastrophically dangerous, as it bypasses normal infection barriers and virtually guarantees HIV transmission if one user is infected. Unlike standard needle reuse, which already carries high risks, bluetoothing involves the direct exchange of blood itself.
This shocking practice is now a defining feature of the Fiji HIV epidemic. Preliminary Ministry of Health data from 2024 show that around half of newly diagnosed cases linked to ART were contracted through injecting drug use. RNZ further reported that nearly 48% of new cases last year came directly from injection practices. The link between bluetoothing and the surging outbreak is undeniable.
Explosive Growth in New Cases
The numbers illustrate just how quickly the HIV crisis in Fiji escalated:
- 2014: About 500 total cases nationwide.
- 2019: New cases begin to rise steadily but remain in the low hundreds.
- 2023: A few hundred new diagnoses—concerning but not yet overwhelming.
- Jan–Sep 2024: Already 1,093 new infections recorded.
- Full year 2024: 1,583 new infections, a 281% increase in just one year.
UNAIDS estimates that the country has seen a ten-fold increase since 2014. Such explosive growth makes Fiji an outlier in the Pacific and positions it as a potential epicenter of a wider regional epidemic. Officials themselves admit that the outbreak has outpaced every existing prevention measure.
Testing, Treatment, and Prevention Gaps
The Fiji HIV crisis is magnified by serious shortcomings across the health system:
- Awareness gap: Only 36% of people living with HIV in Fiji know their status, leaving a large reservoir of undiagnosed cases fueling silent transmission.
- Treatment gap: Just 24% are receiving ART, far below the global average.
- Testing delays: Some clinics report waiting times of up to 22 days for HIV test results.
- Medication shortages: ART stockouts have occurred because the system underestimated the scale of new diagnoses.
- Stigma: Cultural taboos around drug use and HIV create fear and silence, worsening the outbreak.
These combined factors have left Fiji in a reactive stance—struggling to catch up rather than staying ahead of the epidemic curve.
Why Harm Reduction Matters Now
Public health experts are clear: harm reduction works. Needle–syringe programs, safe disposal systems, opioid substitution therapy, and hepatitis C screening have slashed HIV transmission rates in other regions.
Yet Fiji has none of these interventions in place. UNAIDS calls their introduction “urgent and unavoidable.” Without them, the Fiji HIV crisis will continue spiraling upward.
Even worse, misinformation fuels bluetoothing. Many young users falsely believe that sharing blood is less risky than sharing syringes. In reality, it is far deadlier. Community groups argue that prevention campaigns must explicitly target this misconception if Fiji is to reverse course.
Voices from Experts and Officials
The outbreak has drawn sharp responses:
- UNAIDS Pacific Director: “They’re not just sharing needles, they’re sharing blood. This practice has accelerated the Fiji HIV epidemic at an alarming pace.”
- Fiji’s Ministry of Health: Launched a 90-day plan to expand ART supplies and testing, but critics say progress remains slow and underfunded.
- Civil society groups: NGOs like the Fiji Network for People Living with HIV stress that stigma is the single greatest barrier to ending the epidemic.
- Community leaders: Some chiefs and pastors have begun speaking out, but taboos still limit open conversation.
These voices reflect a growing consensus: without systemic reform, the Fiji HIV crisis will only deepen.
Global and Regional Stakes
The Fiji HIV outbreak is not just a domestic issue. UNAIDS warns that the entire Pacific region is at risk if Fiji’s epidemic is left unchecked. Trafficking routes that run through Fiji could spread high-risk behaviors to Tonga, Samoa, and other nearby states, where health systems are equally fragile.
Globally, the outbreak is a reminder of how fast epidemics can accelerate when harm reduction is ignored. The economic toll is also rising: longer hospital stays, surging ART costs, and lost productivity threaten Fiji’s fragile economy. For a country dependent on tourism and remittances, the consequences of an unchecked Fiji HIV crisis could be devastating.
The Road Ahead: Urgent Steps for Containment
Health experts outline a clear set of interventions to stop the epidemic:
- Launch needle–syringe programs immediately, with safe disposal systems.
- Expand rapid testing across urban and rural areas, with same-day ART initiation.
- Directly address bluetoothing in public campaigns, highlighting its extreme danger.
- Engage leaders—traditional, religious, and civic—to dismantle stigma.
- Strengthen ART supply chains to avoid further stockouts.
- Provide youth-friendly services that address addiction, mental health, and peer influence.
If these steps are implemented at scale, the HIV crisis in Fiji could be contained within the next few years. Delay further, and Fiji risks becoming the epicenter of a Pacific-wide epidemic.
Internal Links
- OpenAI’s $500B Valuation Redefines the Future of Artificial Intelligence
- Cybercrime Fight: Police Use Open-Source Tools as Mahama Warns Scammers
External Links
UNAIDS – Fiji HIV outbreak declared (July 2025)
ABC News – Fiji scrambles to contain HIV outbreak driven by “bluetoothing” (March 2025)