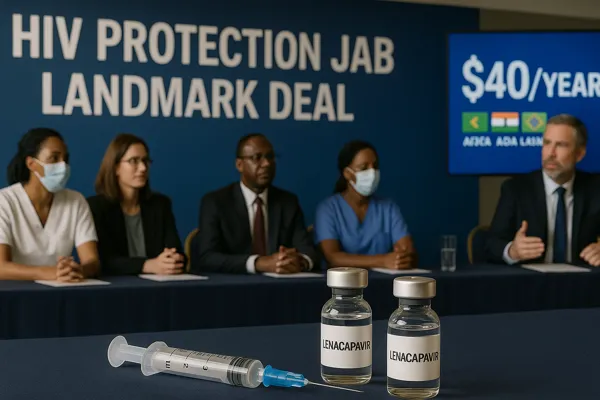
The global campaign against HIV has received a major boost after Gilead Sciences announced a landmark licensing deal that will make the HIV protection jab — the long-acting injectable lenacapavir — affordable in 120 low- and middle-income countries by 2027.
The decision has been hailed as a potential game-changer in global health. For decades, experts have warned that despite progress in antiretroviral therapy, millions remain at risk because they lack affordable access to prevention. The HIV protection jab, which is administered only twice a year, could transform how communities protect themselves against infection.
Currently, the U.S. price of the branded drug, Yeztugo, is an eye-watering $28,000 per year. Under the new deal, generic versions will be available for just $40 annually, one of the sharpest price reductions in HIV prevention history.
HIV Protection Jab Breakthrough Explained
How the HIV Protection Jab Works
The HIV protection jab contains lenacapavir, a first-in-class capsid inhibitor that prevents HIV from entering and multiplying in human cells. Unlike oral PrEP pills, which must be taken daily, lenacapavir is administered once every six months through a subcutaneous injection.
This long-acting design solves one of the biggest obstacles in prevention: adherence. Studies show that while daily PrEP is highly effective, many patients — especially in low-resource settings — struggle to maintain strict daily regimens. The HIV protection jab provides a more reliable, discreet, and convenient alternative.
Who Will Benefit Most
The HIV protection jab is expected to make the greatest impact in:
- Sub-Saharan Africa, where adolescent girls and young women face high infection rates.
- Marginalized groups such as sex workers, LGBTQ+ communities, and migrant workers.
- Rural areas where access to daily pill distribution has been inconsistent.
By reducing the need for frequent clinic visits, the jab could empower at-risk populations to stay protected with less stigma.
Why the HIV Protection Jab Deal Matters Globally
A Turning Point in HIV Prevention
The licensing agreement allows generic manufacturers — including Dr. Reddy’s Laboratories and Hetero in India — to produce low-cost versions of the jab. This deal was facilitated by organizations such as Unitaid, the Clinton Health Access Initiative (CHAI), and the Bill & Melinda Gates Foundation, which negotiated access and pledged support for early production.
Experts see this as the most significant opportunity since the rollout of antiretroviral therapy (ART) in the 1990s, when generic competition helped slash treatment costs and saved millions of lives.
Price Comparison: $28K vs $40 HIV Protection Jab
- Current U.S. cost: $28,218 per year
- Future generic cost: $40 per year
Such a dramatic price cut means governments and aid programs can cover far more people within existing budgets.
Challenges Facing the HIV Protection Jab Rollout
The 2027 Timeline Gap
The most immediate concern is the waiting period. Generic production will not begin until 2027, leaving a critical two-year window where at-risk populations remain unprotected.
Countries Excluded From the Deal
While 120 countries will benefit, several middle-income nations — including some in Eastern Europe, Latin America, and Asia — are excluded from the voluntary licensing list. This means millions may still face prohibitively high prices unless separate negotiations succeed.
Financing and Infrastructure Hurdles
Even at $40 per year, large-scale distribution requires:
- Cold-chain logistics to store and transport the jab.
- Training for healthcare workers to administer biannual injections.
- Community outreach to overcome stigma and encourage uptake.
Without adequate financing from donors like the Global Fund and PEPFAR, rollout may stall in countries most in need.
How the HIV Protection Jab Could End the Epidemic
UNAIDS Projections
UNAIDS estimates that if the HIV protection jab is widely adopted, it could prevent millions of new infections by 2030. In regions like southern Africa, where HIV prevalence remains high, uptake could reduce transmission by up to 80% in high-risk groups.
A Step Toward Ending AIDS as a Public Health Threat
The World Health Organization has set a target of ending AIDS as a public health threat by 2030. Experts believe that the HIV protection jab, combined with scaling up ART and community-based testing, could finally make this target achievable.
Role of Unitaid and CHAI in HIV Protection Jab Rollout
Unitaid and CHAI will help coordinate distribution channels, negotiate procurement prices, and assist governments in integrating the jab into national HIV prevention strategies.
Broader Impact on Global Health Equity
The HIV protection jab deal highlights broader issues of fairness in global health. For years, lifesaving medicines were priced beyond reach in poorer nations, prolonging epidemics that could have been prevented. By licensing generics, Gilead has responded to mounting pressure to prioritize access over profit.
Public health advocates say the deal sets a precedent for future negotiations involving treatments for tuberculosis, malaria, and cancer. It also raises questions about how quickly breakthrough medicines should be made accessible to all, not just wealthy markets.
Internal Links
- WHO issues new clinical guidelines for mosquito-borne diseases
- UN World Food Programme warns of aid collapse in Nigeria
- Understanding Uterine Fibroids: A Hidden Threat to Women’s Health