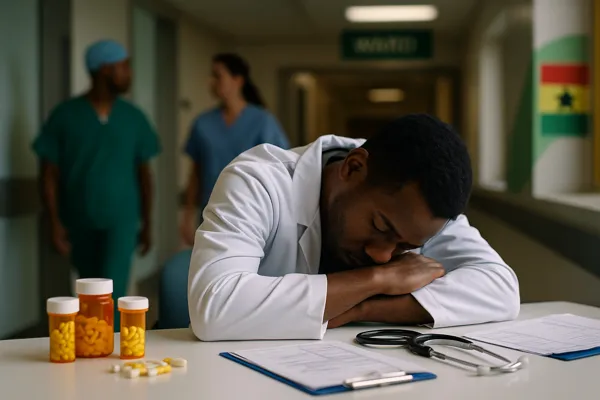
Ghanaian Doctors Mental Health crisis is deepening, with the Medical and Dental Council (MDC) in Accra, Ghana — September 18, 2025, sounding alarm bells over rising psychiatric disorders and substance abuse among practitioners. Many doctors are struggling with depression, schizophrenia, and drug dependency, exposing a hidden challenge in Ghana’s healthcare system—one that threatens both medical professionals and the patients they serve.
The Scope of the Crisis
The latest report from the MDC highlights the alarming scale of the Ghanaian Doctors Mental Health challenge. Increasing numbers of doctors are battling mental health conditions such as depression, anxiety, schizophrenia, and personality disorders. Alongside these psychiatric issues, substance abuse is rising sharply, with some practitioners misusing powerful medications including tramadol, morphine, pethidine, and even heroin.
While mental illness and addiction affect all professions, the risk for doctors is amplified by stressful working environments, easy access to controlled substances, and the stigma that prevents many from seeking timely help. This double burden leaves healthcare workers vulnerable, while putting patients at risk of receiving unsafe treatment.
(Related: Cardiovascular Disease Awareness)
Why Ghanaian Doctors Are at Risk
Several systemic pressures push doctors toward burnout and breakdown. Experts point to four main factors that make the Ghanaian Doctors Mental Health crisis worse:
- Heavy workloads: Ghana has fewer than 4,000 practicing doctors serving a population of 34 million. The result is extreme patient-to-doctor ratios, long shifts, and frequent overtime.
- Poor working conditions: Understaffed hospitals, inadequate medical supplies, and overcrowded wards compound the stress.
- Financial stress: Despite their years of education and high responsibility, many doctors report frustration with modest salaries that do not reflect their workload.
- Stigma and fear: Admitting to psychiatric struggles often carries a perception of weakness. Many doctors remain silent until their conditions spiral out of control.
Dr. Kwabena Osei, a psychiatrist in Accra, explains:
“When doctors struggle with mental illness or addiction, they face a double stigma—as patients and as professionals expected to be strong. Many delay care until it’s too late.”
Schizophrenia and Severe Disorders: A Contested Statistic
One controversial element in the MDC’s findings is the claim that around 30% of affected practitioners exhibit signs of schizophrenia. While some health experts argue this figure may be exaggerated compared to global prevalence rates, its inclusion highlights the severity of the Ghanaian Doctors Mental Health problem. Even if the statistic is overstated, the fact that schizophrenia is reported at all within a professional group signals a systemic failure to support vulnerable practitioners.
(External: Lancet – Physician Burnout and Mental Health)
Substance Abuse Among Doctors
Another dimension of the Ghanaian Doctors Mental Health crisis is substance abuse. The MDC report underscores rising dependency on both prescription and illicit drugs. Doctors, often under intense pressure, sometimes turn to stimulants for energy or opioids for escape.
Commonly abused substances include:
- Tramadol – widely available, often misused for energy and alertness.
- Morphine and Pethidine – opioids used in hospitals but sometimes diverted for personal use.
- Heroin – less common but reported among certain practitioners.
This trend mirrors global findings. The World Health Organization has consistently warned that healthcare professionals face heightened risks of substance abuse because of access to medications and high levels of workplace stress.
(External: WHO – Mental Health at Work)
The MDC’s Response
To address the growing Ghanaian Doctors Mental Health crisis, the Medical and Dental Council has set up a Practice Committee and a Health Assessment Panel, both tasked with evaluating doctors suspected of impairment.
Key steps include:
- Confidential screenings – early detection of psychiatric or substance use issues.
- Mandatory treatment – rehabilitation or psychiatric care before returning to practice.
- License suspensions – temporary removal from practice for unsafe practitioners.
- Rehabilitation pathways – around 80% of doctors who seek treatment early can return to safe practice.
These measures balance patient safety with professional recovery, though critics say enforcement remains inconsistent.
(Related: Student Mental Health 2025)
Patient Safety at Stake
The Ghanaian Doctors Mental Health problem is not only personal but systemic. Impaired doctors risk misdiagnosis, surgical errors, or improper prescriptions—mistakes that could cost patients their lives.
Civil society groups and advocacy organizations are now demanding reforms, including:
- Wellness programs inside hospitals.
- Anonymous helplines for doctors to seek support.
- Integration of mental health care into medical licensing requirements.
International Comparisons
The Ghanaian Doctors Mental Health situation is part of a wider global crisis. In the UK, up to 30% of doctors report depression or anxiety symptoms. In Nigeria, substance abuse among health professionals is steadily rising. In the US, suicide rates among doctors are significantly higher than in the general population.
These comparisons show that Ghana is not isolated, but the challenge is intensified by the country’s limited mental health resources and the heavy strain on its healthcare system.
(External: MyJoyOnline – MDC Findings)
The Way Forward
To combat the Ghanaian Doctors Mental Health crisis, experts recommend a multi-layered approach:
- Invest in infrastructure: More psychiatrists, psychologists, and rehabilitation centers.
- Create safe reporting channels: Confidential systems for doctors to seek help without career repercussions.
- Promote workplace wellness: Better working hours, mandatory breaks, and peer support groups.
- Reduce stigma: Public education campaigns and professional training to normalize mental health care.
(Related: Opioid Abuse Ghana Youth)
Conclusion
The Ghanaian Doctors Mental Health crisis is not just about doctors—it’s about the sustainability of Ghana’s entire healthcare system. If practitioners are overworked, depressed, or battling addiction, patient care inevitably suffers. The MDC’s call to action is a reminder that the health of doctors and the health of a nation are inseparable.